The 2015 Global Maternal and Newborn Health Conference (GMNHC2015) holds a key position in the definition, design and implementation of the Sustainable Development Goals for the health and well-being of pregnant women and their newborns. In a world where women in sub-Saharan Africa and South Asia are 14 times more likely to die as a result of pregnancy than women in high-income countries, equity must serve both as the ethical platform of engagement and the ultimate goal.
Considering the long duration of siloed efforts in global maternal, newborn and under-five morbidity and mortality, critical reflection on the global, national and local dynamics that allow this inequity to persist is needed. GMNHC2015 is an optimal setting to facilitate equity by “replacing concepts of charity with concepts of justice”.[i]
It may be time for the maternal, newborn and child health community to accelerate the processes of disruptive innovation. What is disruptive innovation? It is a “fundamental shift in the paradigm or dynamics of use of a product or service through ‘innovation that is disruptive (by) allow(ing) a whole new population at the bottom of a market access to a product or service that was historically only accessible to consumers with a lot of money or a lot of skill.’ Such transformations turn complicated services into ones that are easier to access and use, opening up new markets that were not being served.”[ii]
Examples of disruptive innovation include personal computers disrupting dominance of mainframe computers, cell phones disrupting dominance of fixed-line phone systems, and
group practice medical clinics replacing traditional single-physician offices in high-income countries. The expansion of cesarean and pelvic surgery skills, along with integration of prolapse and incontinence services into obstetric fistula services, represent similar such innovation in the realm of maternal and newborn health in non-wealthy countries. Equity requires sustainable transformations through efficiencies captured in economies of fiscal scale and clinical scope, as illustrated in the potential extrapolations of the SEED assessment model originally designed for family planning programs.
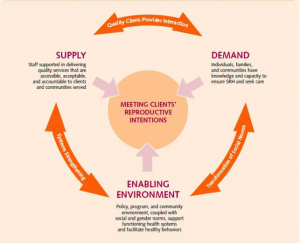
As GMNCH 2015 embraces attention to quality of care, might we also include quality client-provider interaction that embraces systematic engagement of maternal and newborn quality assurance/improvement implementation and monitoring on a broad scale? One such program is The Council for Health Service Accreditation of Southern Africa that accredits private clinics, private hospitals and public hospitals in Southern, Central, East and West Africa. This program uses a list of indicators that underpin national quality assurance and improvement policy in many of the countries where this organization is active.
Let us work within GMNHC2105 find a way to improve health worker density, reward and retention, operative delivery and newborn resuscitation skills and supply chain deficits that plague the progress of health care practice in non-wealthy nations.
Integration at every level, from perspective to programming, is fundamental to the implementation of the SDG agenda. GMNHC2015 is an ideal venue to transform liaisons between governmental and non-governmental stakeholders and each country’s academic institutions and professional associations for obstetrics/gynecology, pediatrics, anesthesia, midwifery, nursing, mental health and general surgery. GMNCH 2015 is also an ideal venue to create viable liaisons between governmental and non-governmental stakeholders and each country’s legal, religious, grassroots, education and local leadership toward the health and well-being of every woman and every child on a platform of equity, catalyzed by efficient service integration and effective quality improvement.
[i] Tifft, Sara. Taking action to ensure access to contraception: new technologies. 2015 (Oct) HR2FP conference, Seattle Washington, USA.
[ii] Christensen, Clayton. Harvard University http://www.claytonchristensen.com/key-concepts


